 More women today survive breast cancer than ever before. But even after a woman and her care team beat the cancer, the disease may leave a reminder of the fight – lymphedema.
More women today survive breast cancer than ever before. But even after a woman and her care team beat the cancer, the disease may leave a reminder of the fight – lymphedema.
Lymph nodes are part of the body’s lymphatic system that carry protein-rich fluid from tissues back to the bloodstream. The body produces four liters of this fluid a day.
But, the lymphatic system can also spread cancer cells through the body. So, when surgeons remove cancer from where it started, they often remove nearby lymph nodes, too, either for biopsy - to make sure they do not contain cancer - or to reduce the risk of the cancer spreading.
Certain radiation therapy and chemotherapy treatments may also affect the lymphatic system.
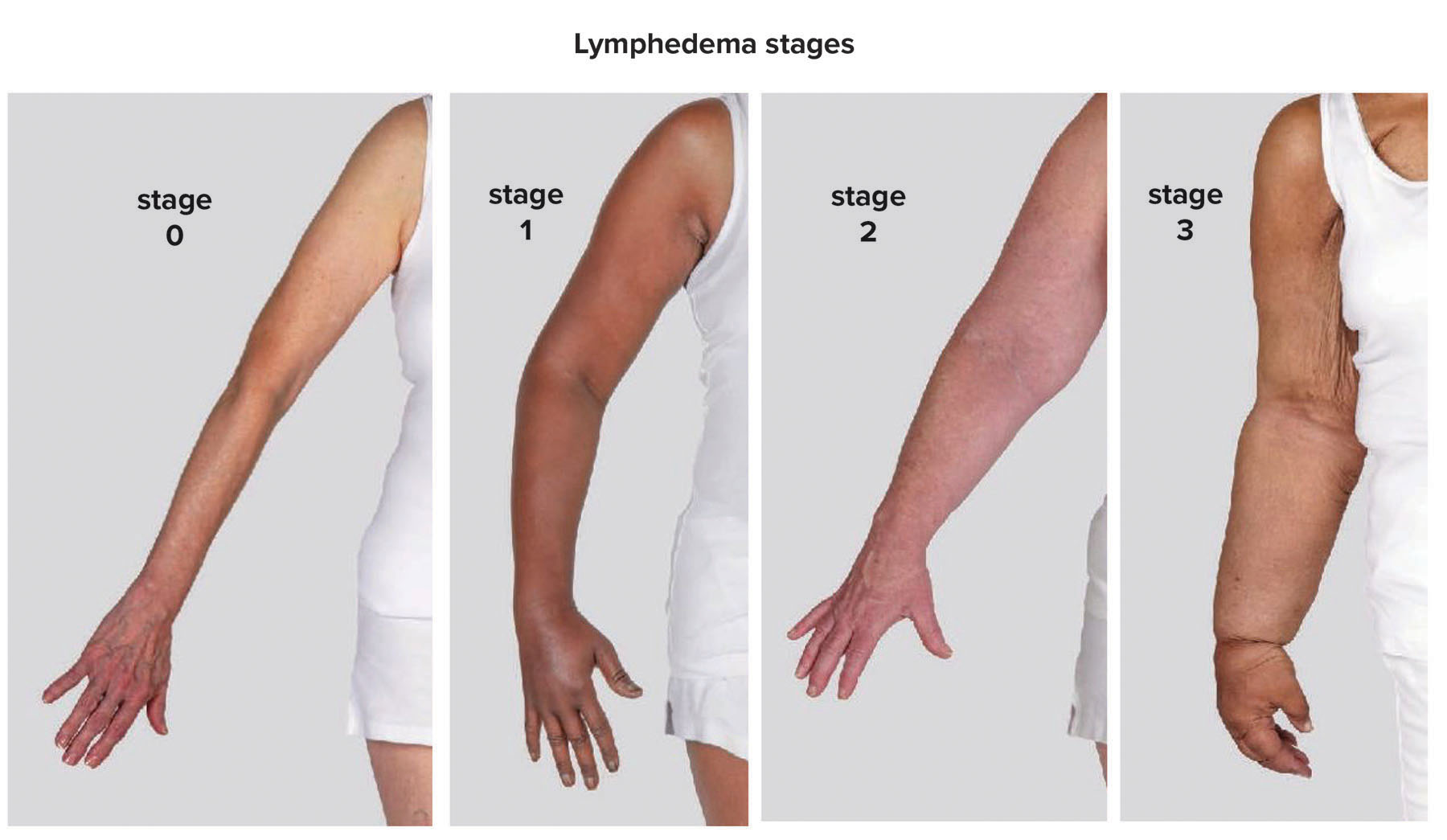
When lymph nodes are affected, it can leave the involved area of the body without a way to drain fluid, because lymph vessels run into “dead ends” where the node used to be. That causes fluid to collect, leading to swelling. After breast cancer treatment, lymphedema can affect the arms, chest and/or trunk of the body.
Lymphedema can also occur in association with other types of cancer, infections, after trauma and due to inherited conditions.
In addition to contributing to a negative body image due to swelling, lymphedema can also lead to medical complications, including skin infections and wound development.
Generally, lymphedema never goes away, but it can be managed. And as with breast cancer, the earlier lymphedema is identified the easier it can be to manage.
Detecting lymphedema
Just as Blessing Health System can treat a woman’s breast cancer, it is there to help the 1-in-3 women who are at risk for lymphedema due to treatment that affects their lymph nodes.
The process often starts with a SOZO scan in the Blessing Breast Center. The SOZO machine looks like a high-tech bathroom scale, but instead of weight, it measures the body’s fluid and tissue status over time to help identify lymphedema earlier in the disease process.
Patient’s whose cancer treatment qualifies for SOZO scanning receive their first scan before treatment begins. This provides a baseline fluid and tissue measurement. Following scans occur during and after cancer treatment is complete and looks for changes in the baseline measurement. The patient is screened every three months for the first three years after their treatment, then every six months for up to two years, and then annually thereafter.
Sometimes, patients will notice the onset of lymphedema themselves.
“They may feel achy. It may also feel full in the affected area of the body, and like pins and needles sometimes, too,’ said Ethan Boren, Blessing Health System occupational therapist and nationally board-certified lymphedema therapist.
 Treating lymphedema
Treating lymphedema
Whether a patient’s SOZO readings increase, or they notice changes in their own bodies, the woman can be referred to Ethan to learn to manage her lymphedema.
“I take measurements. I assess symptoms, including fullness, heaviness, and range of motion,” Ethan explained. “If there is swelling that looks asymmetrical – bigger on one side than the other, we can do manual lymph drainage. We stimulate the lymphatic system in the areas that are affected, moving the fluid to unaffected areas to help promote the body to expel it.”
Therapy can also address fibrosis, the hard tissue that sometimes develops in the affected area.
Ethan says while every patient is different, lymphedema therapy sessions typically take place one-to-three times a week for four-to-eight weeks.
After therapy ends, the patient manages their lymphedema at home for the long-term, including applying compression to the area – either by wearing wraps, or special garments or bandages during certain times of the day – and possibly using a compression pump that does the same thing as manual lymph drainage does, but in the comfort of the patient’s home.
“Lymphedema is something that is always going to be with a person. But you can manage it. It is very manageable,” Ethan stated.
“While lymphedema is easier to treat when caught early, it is not impossible to treat if caught later, either,” he concluded.
For more information on lymphedema, go to blessinghealth.org/treatments/lymphedema.
